Can Lessons Learned from the 1918 Spanish Flu Pandemic Help During the Coronavirus Outbreak?

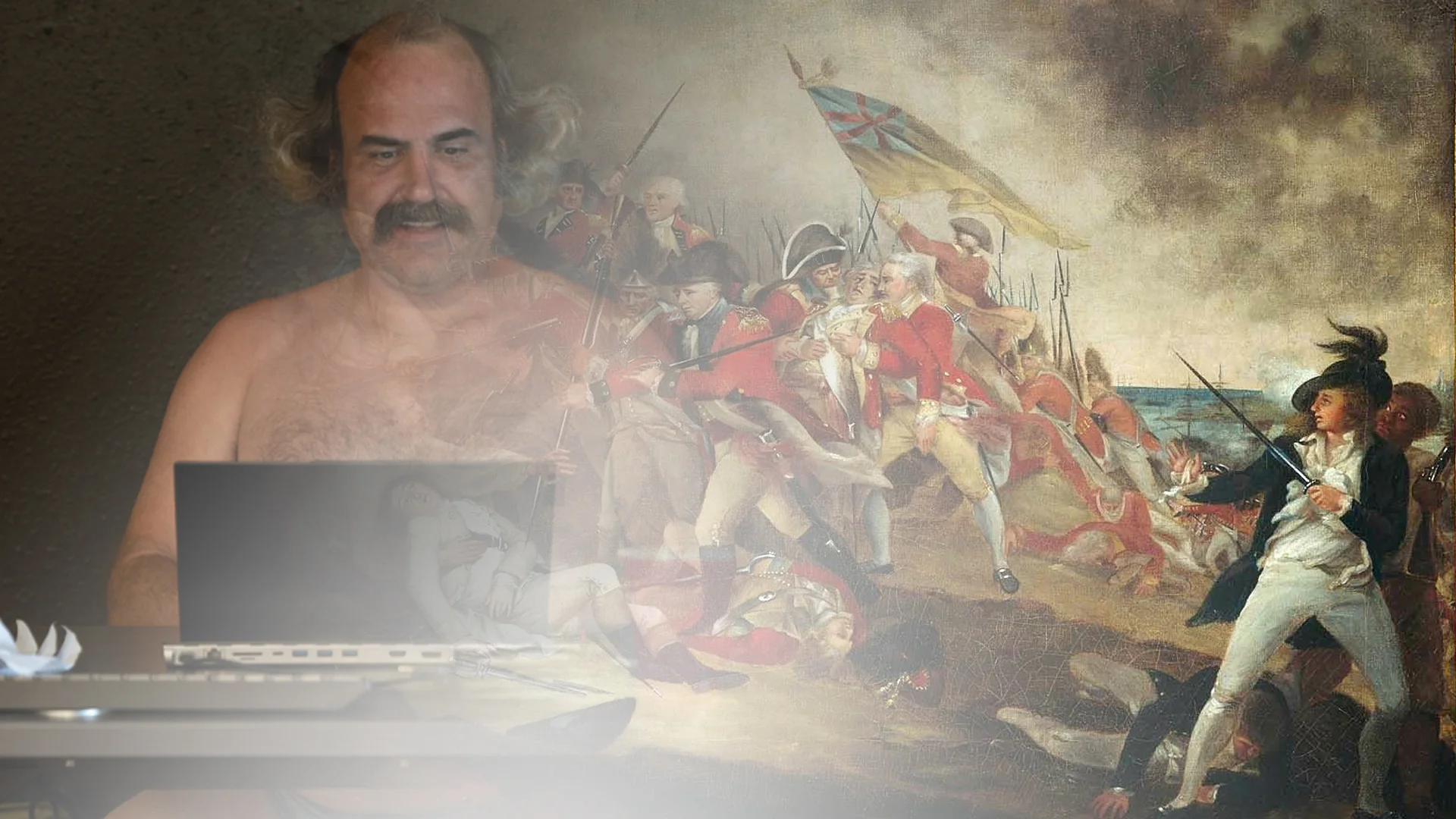
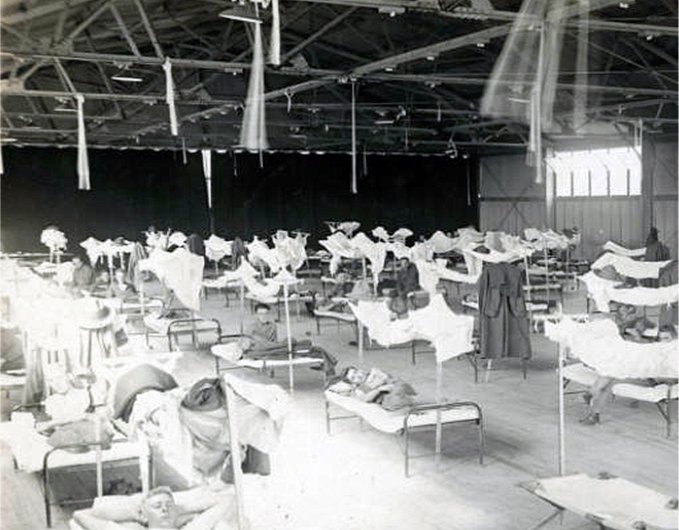
Influenza epidemic in United States. St. Louis, Missouri, Red Cross Motor Corps on duty, October 1918. (National Archives)
The 1918 “Spanish flu” pandemic killed approximately 50 million people, or 3 percent of the global population. Today, it would kill approximately 200 million people if mortality rates remained the same. To put that in perspective, if the United States were infected today with the 1918 influenza, those that contracted the virus would equal the entire population of the Southern region, and North Carolina and Tennessee would have no survivors.
Today, our nation alongside the international community is dealing with a new threat: the COVID-19 pandemic, or more broadly referred to as Coronavirus. It has infected over 585,000 people, killed nearly 27,000, and stopped the global economy in its tracks at the time of this article’s publication.
Although COVID-19 hasn’t reached the death toll of the Spanish flu, there may be lessons we can learn from the last great pandemic a century ago.

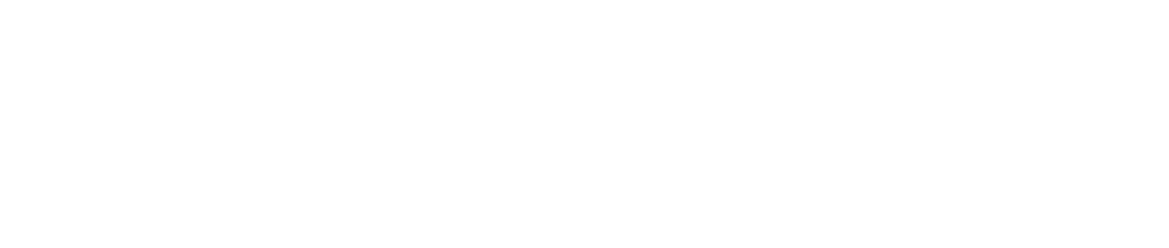
In 2005, a team of researchers from the Armed Forces Institute of Pathology led by pathologist Jeffrey Taubenberger was allowed to sequence the genetic code of the 1918 influenza virus — a crucial step in understanding how a virus operates. The project took tissue samples from the corpses of two American soldiers and one Inuit woman. The woman, named Lucy by researchers, was from an Alaskan village in which 90 percent of its inhabitants died, leaving only eight survivors. But in order to understand the deadliest outbreak in the modern era, it needed to be reconstructed.
The Centers for Disease Control and Prevention (CDC) understood that there would be grave consequences if this virus were to be introduced back into the global population. For that reason, a single microbiologist by the name of Dr. Terrance Tumpey was allowed to study the virus. Tumpey went into the project understanding and accepting that should he become infected, he would be quarantined and denied contact with the outside world.
In addition to the single point of contact, there were no other strains of influenza being studied in the facility to prevent a potential uncontrolled mutation. Stringent Body Substance Isolation standards were put into place, and access to the laboratory was controlled by fingerprint and retinal scan. With these precautions in place, Tumpey conducted his research.
What he found was striking. The 1918 virus was 100 times more deadly than examples of influenza active at the time of testing in 2005. He confirmed that the 1918 virus disproportionately attacked the host’s lung cells, leaving the heart, brain, liver, and spleen relatively intact. In the lungs, however, it produced 50 times the amount of virus as modern common influenza strains. With results like this, it was easy to understand how a virus could kill more than either of the world wars.
Origins of the Virus
The origin of the 1918 Spanish flu is hard to pin down. Reports from Fort Riley on March 4, 1918, are often referred to as the beginning of the outbreak when a cook named Albert Gitchell reported to sick call with a fever, sore throat, and headache. By the end of the day, 107 infected patients were documented. By the end of the month, there were 1,100 infected with 46 deaths caused by influenza or pneumonia secondary to influenza.
Other potential “patient zeroes” (the first documented patients with the disease) were found in a train car full of Chinese workers moving across Canada. China had just been hit with a serious epidemic of upper respiratory infections in the winter of 1917. With World War I raging in Europe, a secret deal with the Allies sent some 94,000 workers of the Chinese Labor Corps to the trenches of France to free up soldiers to fight on the Western front.
According to “The Last Plague: Spanish Influenza and the Politics of Public Health in Canada,” approximately 25,000 of those workers were on train cars moving through Canada en route to Europe, and roughly 3,000 of them were quarantined with flu-like symptoms that were very similar to the Spanish flu. From there the illness took root with Canadian guards, which gave the disease a foothold in North America.
Notably, neither of these potential points of origin were in Spain. The disease became known as the Spanish flu due to widespread reporting in Spain that was uninhibited by wartime censorship seen in the allied nations. Spain remained neutral throughout the global conflicts that have since been referred to as World War I and World War II. Unlike France, Germany, England, Canada, and the United States, the Spanish press widely reported the 8 million infected within its borders in the spring and summer of 1918. Because the infection hit Spain perhaps disproportionately in its early stages (though the censorship of the time prevents accurate figures from being gleaned), and because the news was unencumbered by the conflict across the border, the misnomer stuck.
1918 Influenza Patient Presentation
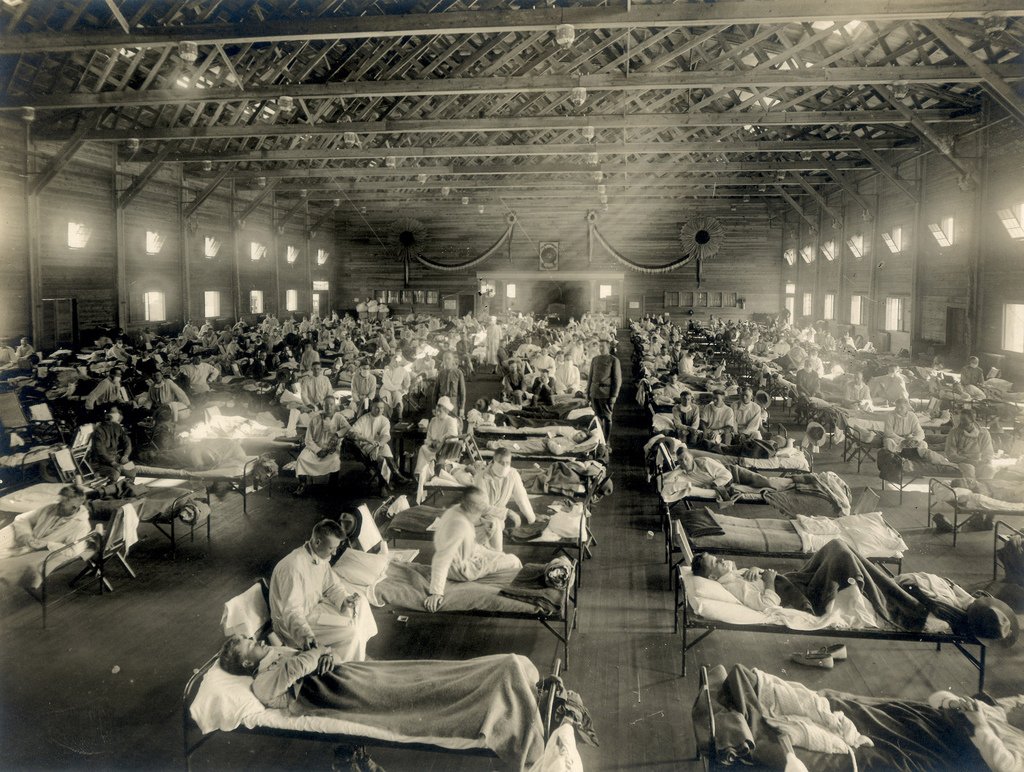
The earliest reports associated with the Spanish flu state that patients complained of body aches, chills, fever, and fatigue. The prognosis was generally good and mortality low. Most deaths from the first wave of Spanish flu were caused by bacterial pneumonia infections secondary to the initial viral influenza.

In the fall of 1918, the world was hit by a much more deadly second wave with deaths occurring within days — sometimes hours — of initial onset. Symptoms differed from the first wave in that patients complained of respiratory issues, often appearing with blued skin — a process called cyanosis — in addition to the previously known symptoms. The second wave is the strain of 1918 influenza that was reconstructed by Dr. Tumpey in 2005. The increased virulence of the second strain resulted in decreased oxygenation as the patient’s lung tissue was destroyed by the potent virus and began to fill with fluid. During autopsy, many patients appeared to have drowned in their own fluid.
The end of World War I in November 1918 resulted in massive troop movements from the disease’s densest concentration in Europe to areas all over the world. The global political climate contributed greatly to the heightened death toll that saw its peak in October, November, and December of 1918. Like Coronavirus today, the 1918 influenza pandemic could be widely attributed to mass global travel.
A third wave of influenza hit the world beginning in January 1919 with equally high mortality rates, but the end of the war minimized the conditions that allowed for the second wave to be so prolific. However, the disease continued on for much of 1919, perhaps even infecting President Woodrow Wilson, who collapsed in Paris during peace negotiations in April of that year.
What was particularly unnerving about the 1918 influenza was that the population that was hit hardest by the infection was not the young and the old like typical infections — it was the seemingly healthiest age group of 15- to 40-year-olds. This likely contributed to a downturn in the global economy as factories and storefronts lost their employees; however, the economic effects are hard to separate from those of the war.
Medical Practices of the Day
In 1918, there was limited understanding of the influenza viral infection. In fact, it was thought to be a bacterial infection at the time. The science of virology was in its infancy, and microscopes of the era were not strong enough to view such tiny sub-organisms. While in the years leading up to the pandemic there were vaccines created to fight diseases such as rabies and tuberculosis, the focus on defeating a bacterium referred to as Pfeiffer’s bacillus, which was wrongly believed to be responsible for the influenza outbreak, distracted the medical community of the time.
A nursing volunteer, Lutiant Van Wert from the Haskell Institute, described what supportive care was like in a letter home to a friend. She described the use of medicines (predominantly aspirin), monitoring temperature, applying ice packs to those with high fevers, feeding the sick, and applying camphorated sweet oils to their chests.
While aspirin was the best medication for fevers at that time, it was relatively new and the dosing was far higher than what would be considered safe levels today. It was normal to give doses in the range of 8 to 30 grams to influenza patients; by comparison, today’s dosages max out at 3 grams per day in divided doses. This may have exacerbated their conditions by inhibiting clotting, causing hyperventilation, and worsening edema — or fluid — in the lungs.
Lessons Learned
With the COVID-19 pandemic currently running its course, what information and practices can we apply today that were learned from the 1918 influenza?
The spread of disease in 1918 closely followed the war effort. Troop movements were necessary as the Allies attempted to defeat the final push made by the Imperial German Army (not unlike the Battle of the Bulge in World War II). Today, while Earth is far from a state of peace, there is less necessity for massive troop movements across oceans and borders. However, tourism accounted for over 1.5 billion international arrivals in 2019, and the economy is much more globally connected than 100 years ago, so it may be more difficult to isolate affected areas from those who have been untouched.

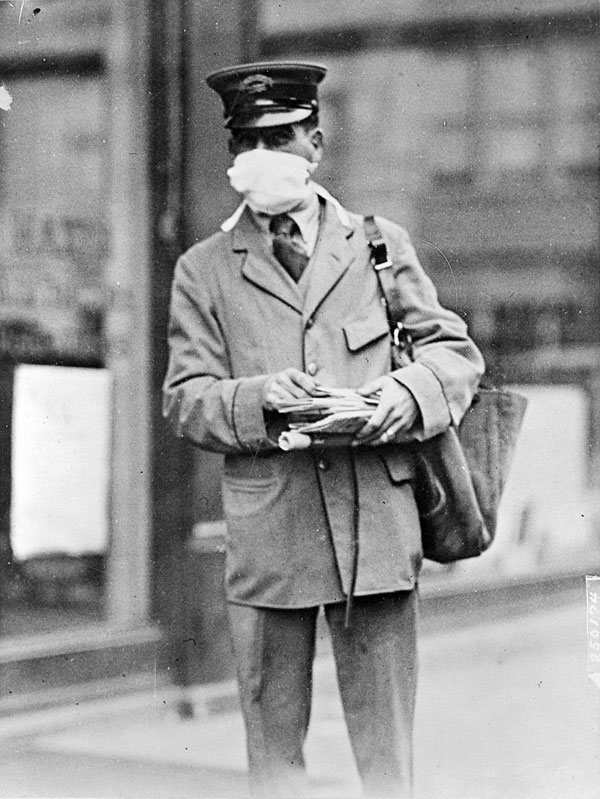
Early testing for infectious disease was impossible during the 1918 Spanish flu. Most diagnoses were made clinically as opposed to using laboratory testing. That meant it was difficult to isolate infected personnel before they had the ability to spread their infection. Fortunately, testing is becoming more available thanks to 21st century medical capabilities. Equally as important, huge strides have been made by the medical community in the understanding and treatment of diseases across the board. We are more capable of managing disease now than ever before.
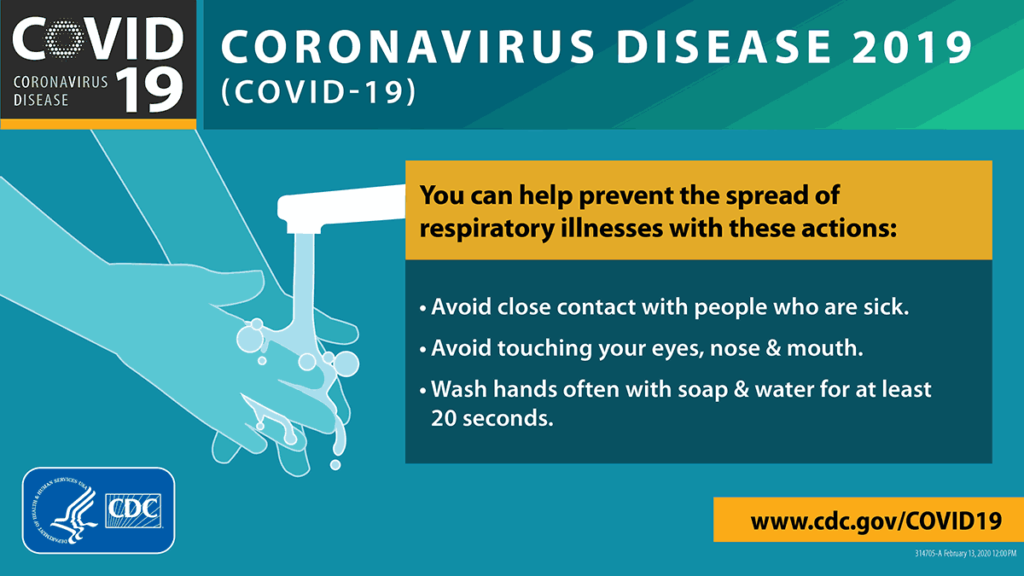
As the saying goes, “An ounce of prevention is worth a pound of cure.” Today, the CDC recommends maintaining good personal hygiene and avoiding interaction with others, if possible, as the best courses of action to minimize the spread of COVID-19.
That being said, it’s important for everyone to remember their humanity despite the threat of sickness. Edna Register Boone was 10 years old when she survived the 1918 pandemic in her home in Alabama. The following is an excerpt from an interview with her:
“One thing that I remember that my father did — there was an open space on one side of our house, I would say the west side, that Papa ploughed up, totally. I don’t know what the measurement was, I’d say fourth of an acre, and planted sweet potatoes. I would say that half of the community lived off of that potato patch. No one was able to go shopping. No one was able to cook. They could bake a few potatoes, even if it was in the fireplace. I knew I had to participate…
… We were like a great big family, you might say. I doubt if we had 200 residents. It brought families closer together. It brought our little town closer together because we all suffered losses, one way or the other, if not through war, then through the epidemic.”

Bryce is a contributing writer at Coffee or Die Magazine, and a former special operations combat medic that served a total of 8 years in the 75th Ranger Regiment and 160th SOAR. He now works as a medical instructor for the Joint Special Operations Medical Training Center, and is also a medical humanitarian aid worker for Earth Mission Asia and the Special Operations Medic Coalition. Bryce has previously been published in Ragged Edge Solutions Med+Blog as well as appeared on the SOM+Cast podcast.
BRCC and Bad Moon Print Press team up for an exclusive, limited-edition T-shirt design!
BRCC partners with Team Room Design for an exclusive T-shirt release!
Thirty Seconds Out has partnered with BRCC for an exclusive shirt design invoking the God of Winter.
Lucas O'Hara of Grizzly Forge has teamed up with BRCC for a badass, exclusive Shirt Club T-shirt design featuring his most popular knife and tiomahawk.
Coffee or Die sits down with one of the graphic designers behind Black Rifle Coffee's signature look and vibe.
Biden will award the Medal of Honor to a Vietnam War Army helicopter pilot who risked his life to save a reconnaissance team from almost certain death.
Ever wonder how much Jack Mandaville would f*ck sh*t up if he went back in time? The American Revolution didn't even see him coming.
A nearly 200-year-old West Point time capsule that at first appeared to yield little more than dust contains hidden treasure, the US Military Academy said.